03/16/2021
Colorectal Cancer & Screening - Frequently Asked Questions
What is Colorectal Cancer?
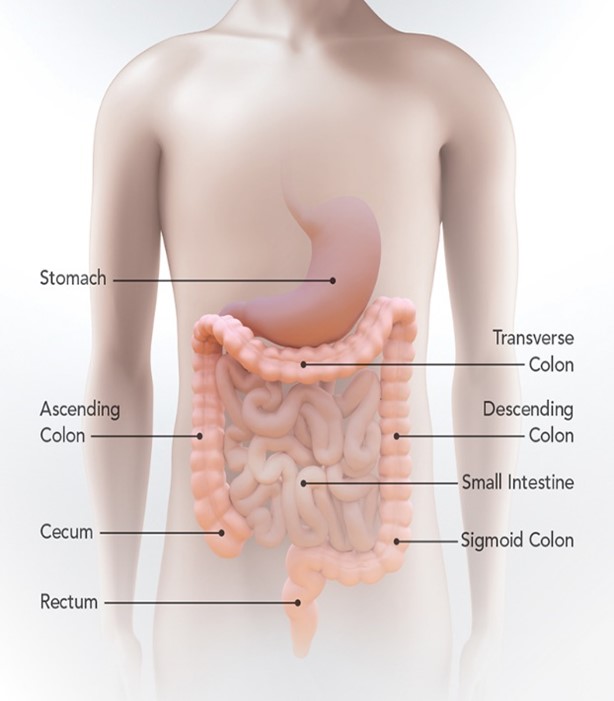
The colon is also known as the large intestine or large bowel and is connected to the anus by the rectum. Colorectal cancer, colon cancer for short, is known to affect these areas. Abnormal growths called polyps can form in the colon or rectum and overtime, can become cancerous.
(https://www.cdc.gov/cancer/colorectal/basic_info/what-is-colorectal-cancer.htm)
What are the guideline recommendations for colorectal cancer screening?
The U.S. Preventative Services Task Force recommends that adults between the ages of 45-75 get screened for colorectal cancer. The task force also recommends that individuals that are younger than 45 with a family history of colorectal cancer and/or colon polyps or have personal history of inflammatory bowel disease be screened as soon as possible. Anyone older than the age of 75 is at the discretion of the individual and their doctor. Any questions as to whether you need to be screened or not should be discussed with your primary care doctor.
(https://uspreventiveservicestaskforce.org/uspstf/recommendation/colorectal-cancer-screening)
What are the risk factors for colorectal cancer?
As you get older, the risk of getting colorectal cancer increases and about 90% of cases are noted in people aged 50 or older. Though it has been shown that individuals younger than 50 have a lower risk of developing colon cancer, recent data has shown that there is an upward trend of colon cancer risk in these individuals.
Other risk factors include:
- History of inflammatory bowel disease, such as Crohn’s Disease or ulcerative colitis
- Family history of colorectal cancer and/or colon polyps
- Certain genetic syndromes such as Lynch Syndrome
- Minimal physical activity
- A diet that is low in fruits and veggies
- A diet that is low in fiber and high in fat
- Obesity or being overweight.
- High alcohol consumption
- Use of tobacco products
How can I reduce my risk of colorectal cancer?
The best way to reduce you risk of colorectal cancer is to get screened per CDC guidelines. Other things that you can do to help is:
- Changing your diet to ensure more fruits and veggies, as well as increasing fiber intake
- Exercise
- Limiting alcohol intake
- Avoiding all tobacco products




What kind of screenings are there?
The American Cancer Society recommends that individuals at average risk start screening at age 45, either with sensitivity tests or with colonoscopy. While the Task Force recommends several screening options, it is best to discuss which option is best for you. Screening options can include:
- Stool Tests - These tests involve obtaining a stool sample and these are sent to the lab to check for specific markers within the stool.
-
Guaiac-based fecal occult blood test (gFOBT) detects blood in stool (an indicator there may be an issue in the colon); to be done 1x/year.
-
Fecal immunochemical test (FIT) uses antibodies to detect blood in the stool; to be done 1x/year.
-
FIT-DNA test combines the FIT test with a test that detects altered DNA in the stool. This test requires an entire bowel movement, rather than a sample and is sent to the lab to see if it detects any cancer cells in it. This test can be done every 3 years.
-
-
Flexible Sigmoidoscopy - This test consists of a short, thin, lighted and flexible tube be inserted into your rectum by a doctor, typically a gastrointestinal (GI) specialist and they check the lower third of the colon in order to check for polyps or cancer. This test is recommended to be done every 5 years (or sooner if recommended by GI) or every 10 years with a FIT every year.
-
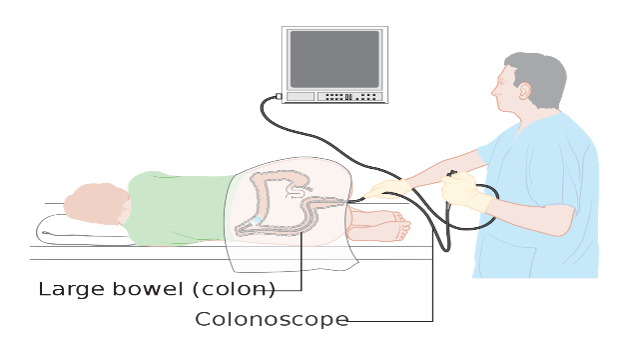
Colonoscopy - While this test is like the sigmoidoscopy, a longer tube is used to survey your entire colon. During this test, the GI specialist will also remove polyps and take samples of tissue for biopsy if needed. Colonoscopy is known to be the gold standard for colorectal cancer screening, since if there are polyps or cancerous cells noted, they can be removed and/or biopsied immediately. This test can be done every 10 years or per sooner per doctor recommendations.
-
CT Colonography - This test uses x-ray and computers to produce an image of your entire colon and the doctor will assess on a screen. This test is recommended every 10 years or sooner per doctor recommendations.
Again, it is best to decide which test is best or right for you through a discussion with your primary care provider!! There are also some tests that your insurance may not cover, which they will also be able to steer you towards.
My primary care provider recommend I get screened for colorectal cancer. Now what?
Now that you have discussed this with your primary care provider and have agreed to screening, they will send a referral to a GI specialist. During your GI specialist appointment, you will have a further discussion regarding your options and what is best for you. After, you will be scheduled for your procedure, either in the GI office or at the hospital.
I know that I need to be screened for colorectal cancer, but I have heard the preparation for a colonoscopy is terrible. What do I need to know?
The preparation or “prep” for colonoscopy or sigmoidoscopy can be unpleasant but is much more tolerable then in years past. There are many different options that you can discuss with the GI specialist. Prep for these procedures consists of cleaning out your bowels, so that the provider to get a better look at your colon. It is imperative that the prep is completed based on your doctor’s instructions. Otherwise, you run the risk of having to redo the prep and the procedure.
I am terrified of getting a colonoscopy, what are the risks involved?
While many people have the same feeling towards colonoscopy, they find that after the procedure is done, the prep was the worst part. While any procedure preformed may have risks, there are minimal with this procedure. Anesthesia is used to sedate for colonoscopy, so with the use of anesthesia, there runs a risk of side effects.
Minor side effects can include nausea, vomiting, chills and confusion. Major side effects can include postoperative delirium or cognitive dysfunction, malignant hyperthermia (in which a fever and muscle contractions come on quickly) or difficulty breathing. These major side effects are extremely rare, however.
(https://www.asahq.org/madeforthismoment/anesthesia-101/anesthesia-risks/)
As far as risks from the procedure itself, risks include infection, bleeding (are the most common) and intestinal perforation (in which the instruments penetrate the colon) can be issues, though they tend to be rare.
(https://www.healthline.com/health/colonoscopy-risks#risks)
Your GI specialist will address any of these questions both at the pre-operative consult, as well as on the day of the procedure. The anesthesiologist assigned to your case will also be discussing risk factors with you on the day of your procedure.
What protocols does Wentworth Douglass have in place to protect me from COVID 19?
During these uncertain times, many people are afraid to come to the hospital for their care, but rest assured, there are many policies and protocols in place to keep you safe. First off, you will be asked to get a COVID screening prior to your procedure. The procedure will not take place unless a negative test result has been noted. Further, all patients and staff are required to wear masks at all times on hospital grounds. For further COVID 19 information, please go to www.WDHospital.org.

(https://www.vcuhealth.org/news/covid-19/face-masks-why-to-wear-them-how-to-clean-them)
For more information, please speak with your doctor or other healthcare provider. More information can also be found at https://www.cdc.gov/cancer/colorectal/.
***All above information obtained at https://www.cdc.gov/cancer/colorectal/, unless otherwise noted.